Microscopic Colitis: Everything You Need To Know
Microscopic colitis is a pathology of the colon, the last section of the large intestine. It is more common in women older than 60 years.
This disease consists of an inflammation of the colon that is only visible at a microscopic level, from which its name is deduced. Two variants are distinguished: lymphocytic colitis and collagenous colitis.
Pathogenesis of microscopic colitis
The exact mechanism by which this pathology occurs is not known. An altered immune response is known to take place in subjects with a genetic predisposition. Therefore, environmental and genetic factors influence.
It has been linked to some molecules of the HLA complex. This system is related to the immune system, having different types of HLA molecules. The DQ2 and DR3 forms are associated with microscopic colitis.
These HLA molecules also influence celiac disease, so it is suspected that the pathogenesis may be related. Environmental factors such as:
- Smoking
- Intestinal infections
- Use of certain medications. Some of the most related are acetyl salicylic acid (aspirin), NSAIDs like ibuprofen, and proton pump inhibitors like omeprazole.
Furthermore, microscopic colitis is associated in more than a third of cases with autoimmune diseases. This supports the theory that an immune alteration is involved in the pathogenesis of this disease.
Another fact that supports this suspicion is that lymphocytes, cells of the immune response, are in greater quantity in the intestinal mucosa of these patients.
Symptoms of microscopic colitis

Although, as we have said, there are two variants of this disease, the symptoms are similar in both variants:
- Chronic diarrhea. Stools are watery and bloodless. Sometimes instead of chronic it follows an intermittent course.
- Urgency or incontinence. Symptoms persist overnight and may be accompanied by abdominal pain and slight weight loss.
As can be seen, the symptoms are nonspecific so other intestinal pathologies such as irritable bowel syndrome and inflammatory bowel disease must be ruled out. It is also advisable to rule out more serious diseases such as colon cancer.
Diagnosis of microscopic colitis
The suspicion of microscopic colitis is established based on the symptoms, increased if it is associated with autoimmune diseases.
Laboratory tests such as stool studies or blood tests can provide information, although they are not diagnostic. Inflammatory parameters may be increased.
An inflammation supposes an arrival of immune cells to the infectious focus, such as neutrophils. These cells have calprotectin and lactoferrin in their cytoplasm, so their presence in the stool can warn of inflammation.
The confirmatory diagnosis is made by two tests:
- Endoscopy (colonoscopy).
- Biopsy.
1. Colonoscopy
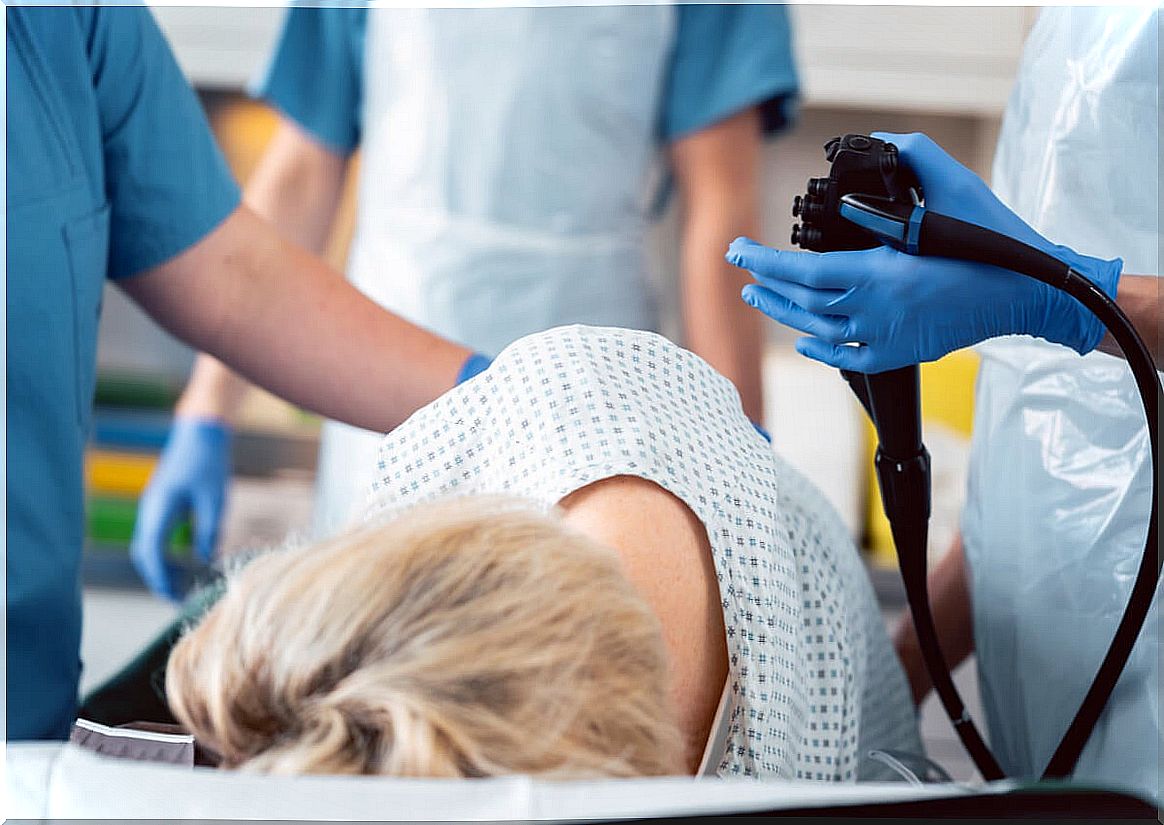
Colonoscopy is an imaging technique that allows you to see the mucosa of the colon directly.
We have said that the alteration of the colonic mucosa in microscopic colitis is not observed with the naked eye. Even so, colonoscopy is indicated to rule out other pathologies and take biopsies that allow histological study.
On some occasions, nonspecific changes may be observed in the intestinal mucosa, such as erythema (reddened mucosa) or edema (mucosa swollen due to the presence of fluid).
2. Biopsy
Once the tissue samples have been taken, their histological study makes it possible to confirm or rule out the diagnosis. The histological criteria for microscopic colitis are:
- Lesion of the epithelium of the colon, the most superficial layer.
- Increased number of intraepithelial lymphocytes.
- Inflammatory cells in the lamina propria. The lamina propria is the layer located under the epithelium. There should be no abscesses or gland abnormalities.
In addition, the microscopic study allows to differentiate the two variants of microscopic colitis:
- Collagenous colitis: in this case a collagen layer will be observed under the epithelium.
- Lymphocytic colitis: the percentage of lymphocytes in the intestinal mucosa must be greater than 20% of the cells.
Treatment of microscopic colitis
At the moment, there is no curative treatment. Currently, the only therapeutic approach is to control the disease symptomatically. It is advisable to avoid the use of drugs that may be related to the disease, as well as to stop smoking.
If it is necessary to use medications, the use of budesonide, a corticosteroid that reduces intestinal inflammation, improves diarrhea, stands out. Cholestyramine can be combined with budesonide if necessary.